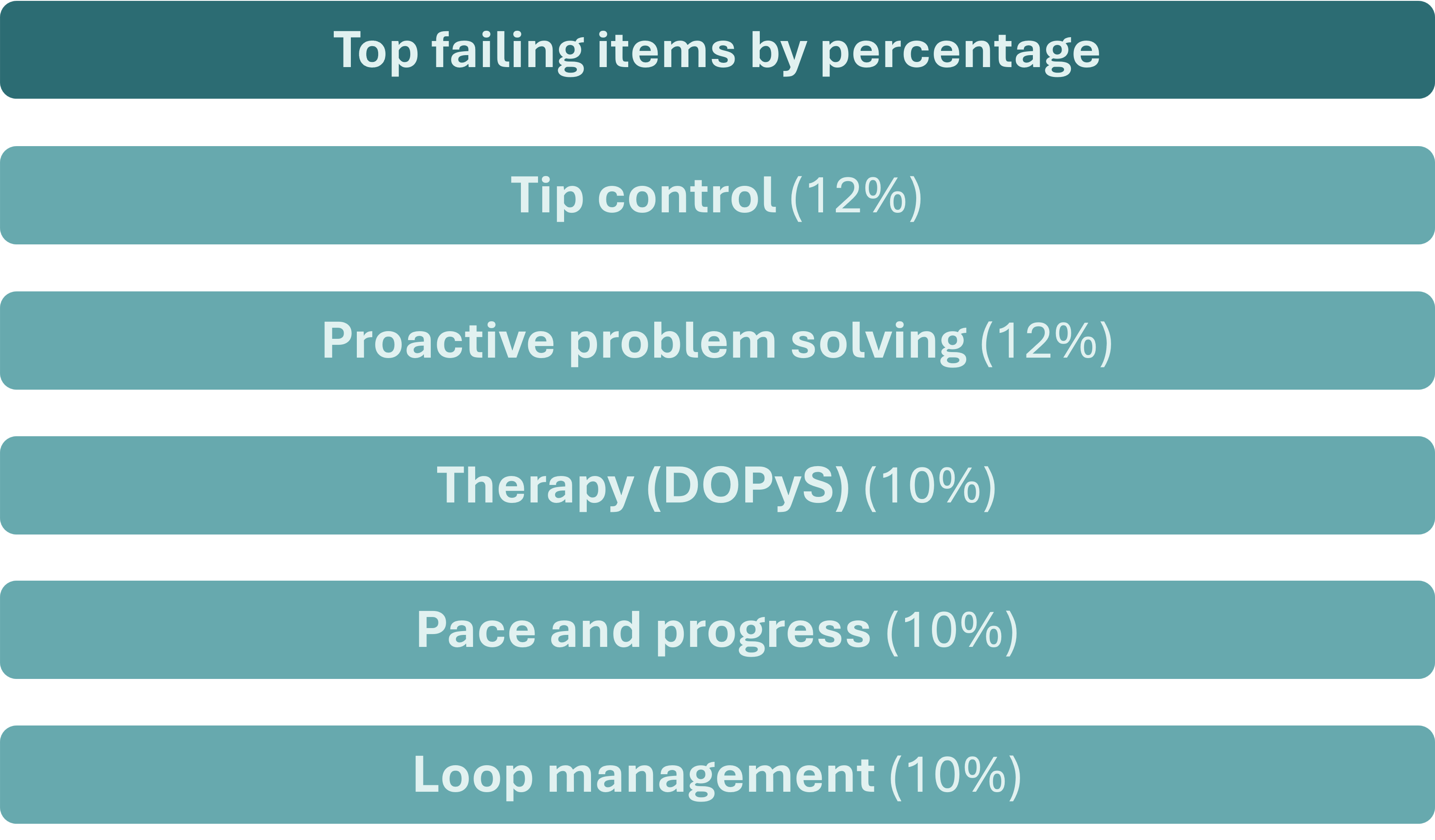
We want all candidates to do well during their assessment. This table shows the fail percentages for each individual item on DOPS forms from 2022 to end of 2024.
Candidates most frequently failed on areas relating to tip control, proactive problem solving, therapy (DOPyS), pace and progress, and loop management from 2022 to the end of 2024:
The below breaks down what is being assessed in each of these areas:
Tip control
- Integrated technique: Combines tip and torque steering to accurately control the tip of colonoscope and manoeuvre the tip in the correct direction.
- Individual components.
- Tip steering: Avoids unnecessary mucosal contact and maintains luminal view, avoiding need for blind negotiation of flexures and 'slide-by' where possible
- Torque steering: Demonstrates controlled torque steering using right hand/fingers to rotate shaft of colonoscope
- Luminal awareness: Correctly identifies luminal direction using all available visual clues, and avoids red outs
Proactive problem solving
- Anticipates challenges and problems (e.g. flexures and loops)
- Uses appropriate techniques and strategies to prevent problems and minimise difficulties and patient discomfort
- Recognition: Early recognition of technical challenges and difficulties preventing progression (e.g. loops, fixed pelvis)
- Management: Can articulate and demonstrate a logical approach to resolving technical challenges, including early change in strategy when progress not being made
Therapy (DOPyS)
- Polypectomy is assessed using DOPyS. Each polypectomy performed will be scored
- To pass the DOPyS for a polypectomy, each of the sections must have an overallscore of ‘achieved’, or where relevant ‘does not apply’
- A full breakdown of the DOPyS scoring system can be found here
Pace and progress
- Takes sufficient time to maximise mucosal views
- Insertion of colonoscope speed adjusted to minimise looping, prevent problems and manage difficulties
- Able to complete both insertion and withdrawal at pace consistent with normal service lists, adjusted, depending on difficulty of procedure
- Extent of examination is appropriate to the indication
Loop management
- Uses appropriate techniques (tip and torque steering, withdrawal, position change) to minimise and prevent loop formation
- Early recognition of when loop is forming or has formed
- Understands and can articulate techniques for resolution of loops
- Resolves loops as soon as technically possible, to minimise patient discomfort and any compromise to scope function
- Recognises when loop resolution not possible and safely inserts colonoscope with loop, with awareness and management of any associated patient discomfort
Please review the full DOPS assessment form to help guide you as to what the assessors will be looking for in each of these areas. This will help you prepare for your assessment and give you the best chance of successfully gaining accreditation. If you undertake polypectomy during your assessment, then your polypectomy skills will be assessed using the DOPyS assessment form.